This is an interesting question that many people are eager to talk about. In this blog post, I will go through what happens to the human body after death in a scientific manner.
NOTE: This is still a work in progress. This requires a lot of reading and I hope to complete this within the next two months.
rrefer to this https://www.slideserve.com/azize/post-mortem-changes-powerpoint-ppt-presentation
Quick Overview
Most people think that death is a single moment. One second you are alive, the next you are not! Scientifically, death is NOT a single event – It’s a chain of phsyiological events where each event leads to the next like dominoes.
It usually begins with cardiac death, which occurs when the myocardium fails to contract effectively (also called cardiac arrest). When the heart stops, the cariac output will be zero, resulting the cardiac perfusion to fall to zero. Without the systemic circulation, the delivery of oxygen to cells and tissues stop while carbon dioxide accumulates. This will lead to global hypoxemia resulting in tissue hypoxia.
The failed systemic circulation will also result in hypoperfusion of the brain stem. This prolonged ischemia of the brain will result in cerebral hypoxia (potentially even complete cerebral anoxia), neuroglycopenia and many other complications.
This results in (anoxic) ischemic depolarization.
- The Na+/K+-ATPase pump is what maintains the transmembrane gradients of K+ and Na+ ions.
- During ischemia, this pump fails and will result in the loss of the ion gradients.
- This will cause the extracellular K+ cocentrations to increase along with an influx of Na+ and Ca2+ ions into the cell.
- This results in net depolarization of the nueronal membrane.
- This will trigger the release of certain neurotransmitters such as glutamate which can bind to and activate various receptors like the NMDA receptor – which will lead to further Ca2+ influx.
- This will lead to excitotoxic injury of the brain stem.
This will result in the permanent loss of brain functions. This is called “brain death”.
Cardiac arrest might be reversible if intervened quickly with cardiopulmonary resuscitation and/or other advanced cardiac life support techniques. However, it depends on a lot of other factors as well. If the patient is not recuscitated within 2 to 5 (or 3 to 10???) minutes, it would cause irreversible ischemic injury to the brain. After that, even if circulation is restored or maintained artifically, the patient will considered to be “dead”. This is because the medicolegal definition states brain death to be the formal definition of death.
Upon the irreversiblee cease of neuronal activity, the body won’t have the capacity for thought, awareness, or sensation. Your body becomes unconsicous, it will loose it’s reflexes and the ability to react to stimuli. Right after death happens, the body encounters it’s first sign of insensibility, the loss of sensation followed by the loss of voluntary power. The concept of “soul” dies along with brain death as everything we associate with being a “person” disappears completely. YOLO!
If brain death occurs first (before cardiac arrest), it will result in the medullary respiratory centors to fail (dorsal and ventral respiratory groups in the medulla oblongata and the pontine pneumotaxic and apneustic centers to be specific). This will cease the generation of rhythmic impulses to the phrenic and intercostal motor neurons, resulting in the diaphragmatic excursions and intercostal muscle contractions to stop, resulting in apnea. This will then lead to systemtic hypoxia and then hypercapnia, resulting in a severe acid-base imbalance. As cardiac myocytes are now oxygen deprived, they will switch to performing anerobic metabolism, resulting in the formation and accumulation of lactic acid, which will weaken the heart’s contractility. Therefore, it will result in bradychardia and will soon progress in to complete asystole.
Upon brainstem death, the sympathetic nervous system (managed by the rostral ventrolateral medulla) can no longer maintain vascular constriction and will result the vasomotor tone to be lost. The artierioles and venules will dilate systemically, leading to a reduced systemic vascular resistance and venous return. This will cause the arterial pressure to fall, resulting in severe systemic hypotension leading to circulatory collapse.
The Edinger-Westphal nucleus and the oculomotor nerve is what controls the constriction of the sphincter pupillae muscle. As the mid brain fails to function, all of this will fail and result in the pupillary light reflex to be lost. Not only that, the corneal relfex is also lost due to the failiure of trigeminal nerve for sensation and the facial nerve for motor control of the orbicularis oculi muscle. Similiarly, the gag reflex is also lost due to the failiure of sensory input from the glossopharyngeal nerve and motor output from the vagus nerve to the pharyngeal muscles.
The loss of hypothalamic function will stop the body’s ability to perform thermoregulation. Usually, under normal circumstances, the hypothalamus maintains homeostasis based on the input from peripheral thermoreceptors and will initiate to perform a response such as vasodilation, vasoconstriction, shivering, or sweating to stabilize the bodys’ temperature. Once the hypothalamic neurons undergo ischemic necrosis, this autonomic function will completely fail, resulting the body to become poikilothermic. This means the body will passively reach equilibrium to the ambient temperature using basic heat exchange mechanisms like conduction, convection and radiation.
Due to the hypoxia, cellular necrosis will begin eventually through the body. In the mean time lysosomal enzymes will leak out, resulting in autolysis.
There’s another term called “somatic death”. This is the death of the whole body, including cellular death. As discussed above, the brain cells will die within minutes after loss of blood circulation but muscle cells, skin cells, and more popularly, corneal cells might remain viable for hours (depending on environmental factors). This is why corneal transplants and skin grafts can still be harvested from recent dead bodies.
The loss of reaction to stimuli is not only limited to these; it can be seen throughout the whole body. Upon brainstem death, cortical activity ceases, resulting in the inability to perform conscious or voluntary responses, while the loss of brainstem and spinal reflex pathways eliminates even involuntary movements. No motor or autonomic response will be produced from painful or tactile stimuli, and the skeletal muscles will also remain flaccid due to the loss of descending motor control. This generalized unresponsiveness shows complete cessation of CNS activity.
Following brain death and the complete loss of CNS function, the upper and lower motor neurons will not send any impulses to skeletal muscles. This will make them lose their resting contraction and become soft, limp and unresponsive to both voluntary commands and reflex stimulation. This will prevent the muscle tone from being maintained and will result in general muscular flaccidity.
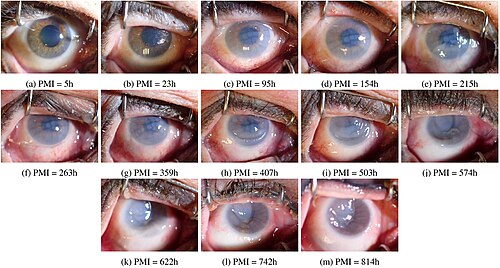
Occular Changes
Within a few minutes, the retinal blood vessels appear segmented or fragmented. It can be seen with an opthalmoscope. It is called the “Kevorkian Sign”. This will appear very quickly after death and will last for approximately an hour.
The pupils will also be dilated mildly.
As blood circulation stops after cadiac arrest, oxygenated blood does not reach the skin anymore. Without capillary perfusion, the pink tone from oxyheamoglobin disappears. This will make the skin turn pale. Since the blood pressure is gone, capillaries won’t refill and the heamoglobin trapped in them will dexoygenate quickly, making it even more pale. This process is called “algor mortis” and usually starts 15-30 minutes after death.
After an hour, the cornea turns hazy.
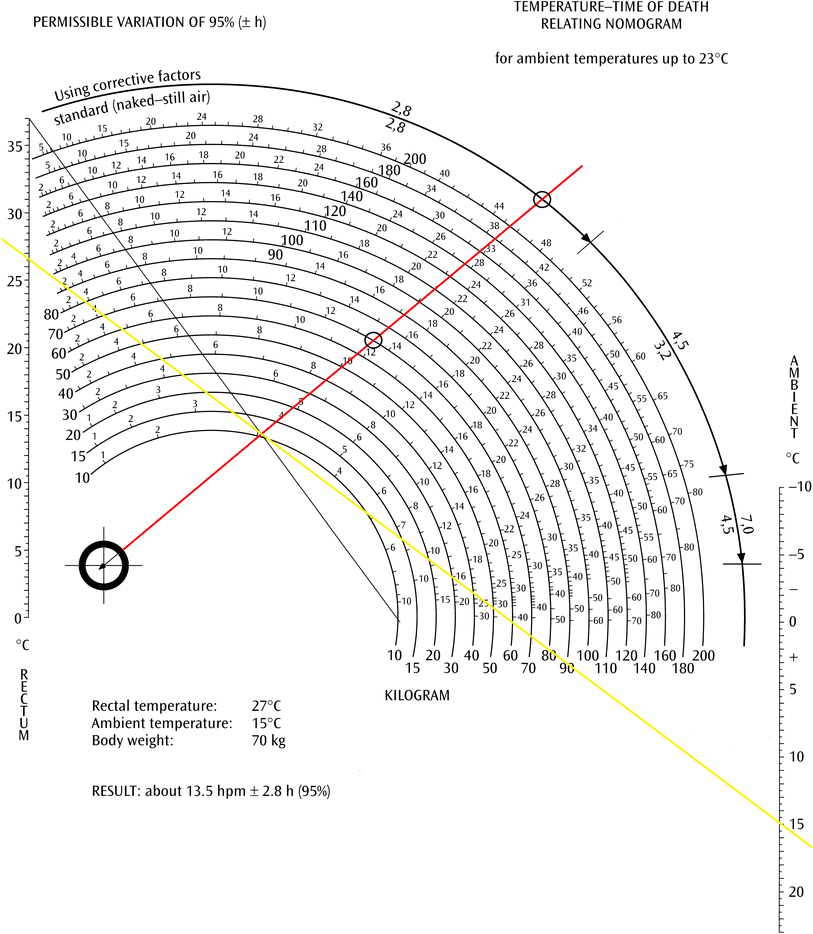
In the mean time, “algor mortis” also takes place. As no metabolic activity takes place, the body will have no way to regulate the temperature. Therefore, the heat dissipates into the environment at about 0.4C to 2C per hour until it reaches equilibreium with the sorrounding environment (0.4C in the winter and 0.7C in the summer). This will of course vary depending on the clothing around the body and the fat content along with a lot of other factors, like wind (which results in heat loss via convection). Some regions of the body will lose heat faster than the others. For example, parts like the face, hands and feet tend to cool more quickly because they have a larger surface area with little fat and musle sorrounding them. Note that fat is insulative. Therefore, the more fat you have, the longer it takes your body to reach equilibrium. Compared to these, the core of the body cools down much slower, specially the thoracic cavity and the abdominal cavity. Algor mortis is an important concept as one of the main time of death estimation in forensic medical studies is based on this. In this case, the rectal temperature is used as it is considered to be the closest to the body core temperature (BCT).
The BCT drop can be graphed and divided into three stages. This graph takes a sigmoid shape.
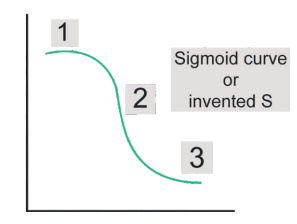
Stage 1 is called the Isothermic phase, stage 2 is called the steep decline phase and stage 3 is called the gradual decrease phase.
Ensure you have a complete understanding of the newton’s laws of cooling before using the Glaister equation to substitute the rectal temperature to calculate the “PMI” (Post Moterm Interval) to adjust the values and/or offsets accordingly.
Below is the glaister equation:
- PMI = (98.7 °F − rectal temperature of the decedent (°F)) / (T)
- Here, T = 1.5 if ambient temperature < 32 °F.
- And, T = 0.75 if ambient temperature ≥32 °F.
This formula is appropriate mostly for environments with typical cooling environments.
Additionally, the Henssge Nomogram is also used to estimate the PMI. Click here to read more about using this accurately.
After two hours, the intraocular pressure will drop from the normal 20 mmHg to zero, increasing the flaccidity of the eye.
After 20 to 30 minutes, the
After 3 to 6 hours, if the eyelids are open, all of the dust present in the atmosphere will get deposited into the sclera, resulting in two brownish triangular shaped opacities to the left and the right of the cornea. This is known as “Tâche Noire Sclérotique”.

Along with that, after approximately 5 hours, the corneal opacity will start increasing.
When I come to putrefication, talk about it here, talk about the eye and how it is resistant to it: https://www.prepladder.com/neet-pg-study-material/forensic-medicine/thanatology-types-of-death-post-mortem-changes
notes
right after death
- muscular flaccidity
- mild dilated pupils
- eyelids usually closed incompletly, resuling in tache noire
hypostatis vs livor mortis vs post moterm lividity seperate out the rectal temperature part and the equations talk only about death talk about other crap later
blanching
livor mortis of internal organs + find images for everything mentioned above livor mortis color (toxicology) tardieu spots
rigor mortis cadaveric spasm their difference
algor
decomposition marbling putrefaction active decay skeletanization mummification
maggot and fly eggs and stuff, durations, images, when
Shortly after death, due to relaxation of muscles, including the iris, the eyes will dilate (pupils grow larger). However, with the onset of rigor mortis, the pupils constrict. They may be unevenly dilated or constricted, and may even appear oval.
autolysis
cover time estimations forensic side of things look at a case study
refer to MI myocardial necrosis from simpsons textbook also about other organs